What is Prone Transpsoas (PTP™)?
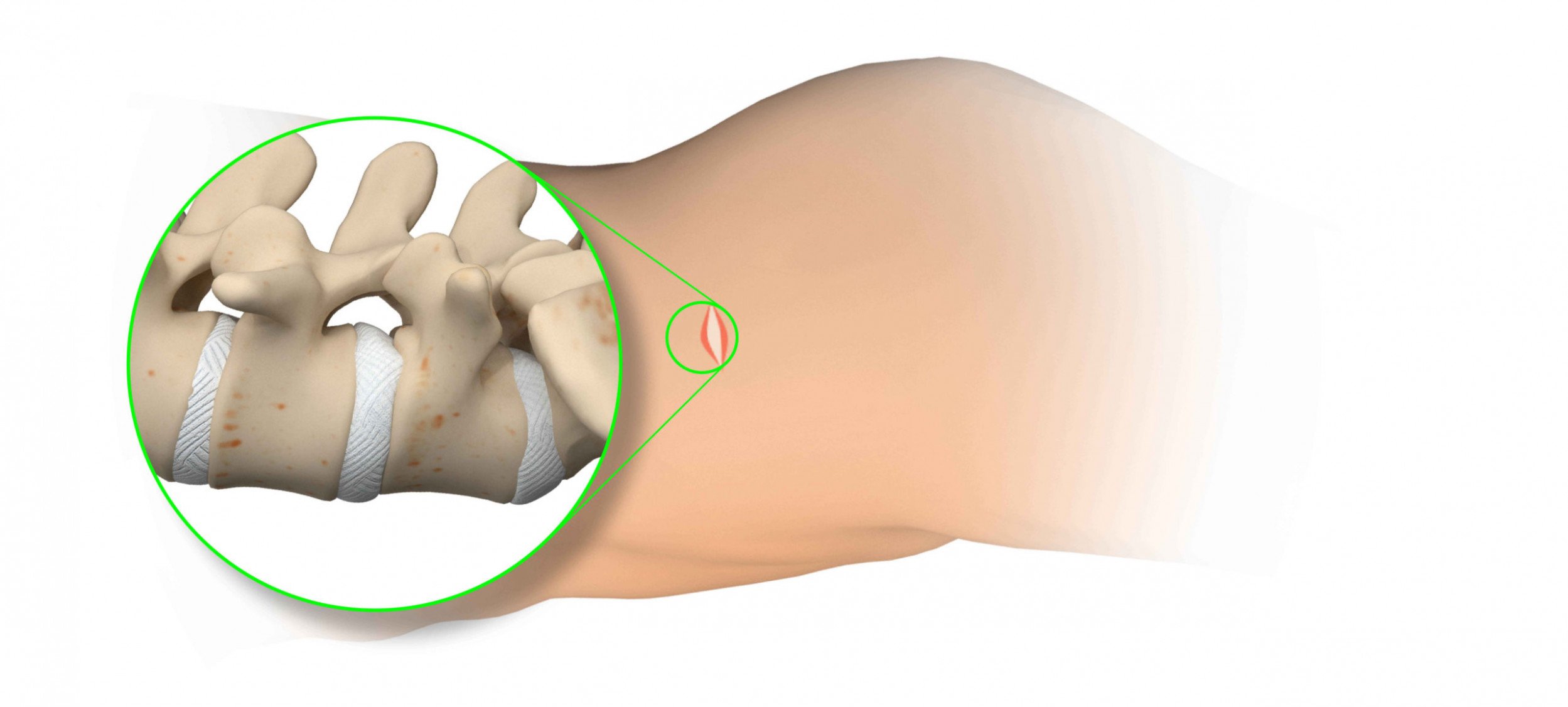
The Prone Transpsoas approach is a minimally invasive spinal procedure where the spine is accessed through a small incision in the side of the body while the patient is in the prone position. The approach allows for the correction of the natural curvatures of the spine to improve overall spinal alignment. This muscle- and bone-sparing procedure leads to less time under anesthesia, less blood loss, shorter hospital stays, and quicker time to walking compared to traditional approaches.1-4
Pathologies addressed by PTP
There are many primary causes of back pain. Some of the problems originate from disc, bone, or ligaments pressing onto the spinal cord or nerve roots.

DEGENERATIVE SCOLIOSIS
Also known as adult onset scoliosis, describes a side-to-side curvature
of the spine caused by degeneration of the facet joints and intervertebral discs which are the moving parts of the spine. This degeneration and resulting spinal asymmetry can occur slowly over time as a person ages. This is a completely different cause of scoliosis from the standard adolescent onset scoliosis.

DEGENERATIVE DISC
DISEASE (DDD)
The natural aging process can cause your intervertebral discs to
lose flexibility, height, and elasticity. Pain may result as an effect of irregular alignment or motion of the spine. If the disc bulges or herniates, the displacement may compress the nerves that run through the spine and cause pain or numbing in the lower back and/or legs.

DEGENERATIVE SPONDYLOLISTHESIS
Degenerative spondylolisthesis is a condition in which a vertebral body slips out of alignment and over the vertebra below it, which can cause instability in the spine and pressure on the local nerves. The condition is usually the result of degenerated discs, but can also result from stress fractures, birth defects, and in rare cases, a tumor or trauma.
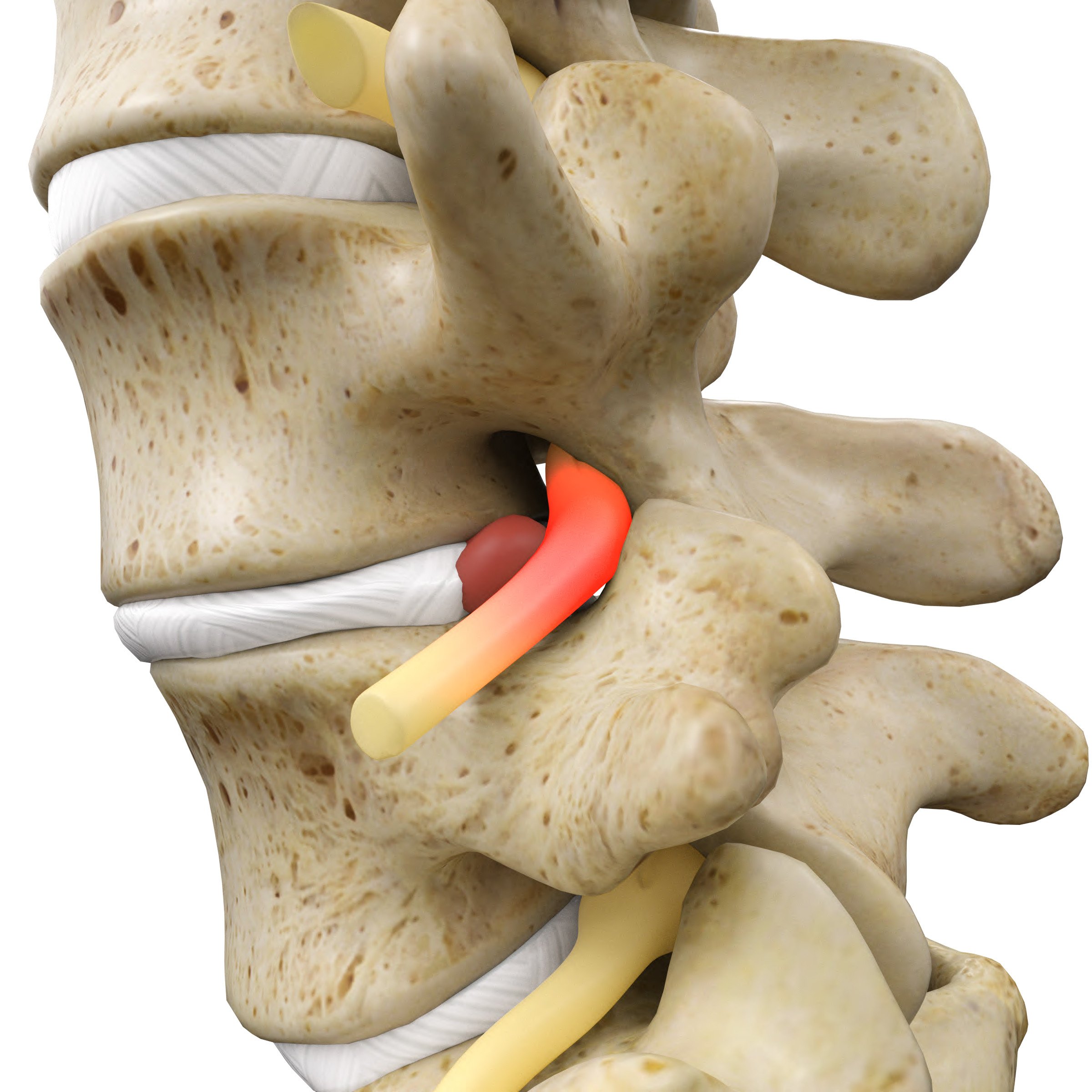
SPINAL STENOSIS
Spinal stenosis is the narrowing of the spinal canal where your spinal cord lies and nerve roots originate. This puts pressure on the cord and/ or nerve roots causing pain and weakness. This condition often arises along with other degenerative changes such as DDD and spondylolisthesis, but can also occur alone or associated with other spinal problems including changes in normal spinal alignment.
1Lehmen JA, Gerber EJ. MIS lateral spine surgery: A systematic literature review of complications, outcomes, and economics. Eur Spine J 2015;24(Suppl 3):S287-313.
2Smith WD, Christian G, Serrano S, et al. A comparison of perioperative charges and outcome between open and mini-open approaches for anterior lumbar discectomy and fusion. J Clin Neurosci 2012;19:673-80.
3Lucio JC, VanConia RB, DeLuzio KJ, et al. Economics of less invasive spinal surgery: an analysis of hospital cost differences between open and minimally invasive instrumented spinal fusion procedures during the perioperative period. Risk Manage Health Policy 2012;5:65-74.
4Ozgur BM, Agarwal V, Nail E, et al. Two-year clinical and radiographic success of minimally invasive lateral transpsoas approach for the treatment of degenerative lumbar conditions. SAS J 2010;4:41–6.
5Guiroy A, Carazzo C, Camino-Willhuber G, Gagliardi M, Fernandes-Joaquim A, Cabrera JP, Menezes C, Asghar J. Single-position surgery versus lateral-then-prone-position circumferential lumbar interbody fusion: a systematic literature review. World Neurosurg 2021;151:e379-86.
6Pesenti S, Pannu T, Andres-Bergos J, Lafage R, Smith JS, Glassman S, de Kleuver M, Pellise F, Schwab F, Lafage V. What are the risk factors for surgical site infection after spinal fusion? A meta-analysis. Eur Spine J 2018;27(10):2469-80.